Best For You
A minimally invasive procedure commonly used to diagnose and treat certain heart conditions is cardiac catheterization. To get to the heart, a thin, flexible tube must be inserted through a blood vessel. With the assistance of the catheter, your physician can carry out some procedures and diagnostic tests on your heart. Most of the time, this procedure is done through the groin or femoral artery. The femoral artery has emerged as the most common method for cardiac catheterization due to its larger size and direct access to the heart. However, the use of the radial artery for cardiac catheterization has significantly increased in recent years. When compared to the femoral approach, the radial artery approach is associated with less bleeding and fewer complications, making it safer for patients.
Benefits of radial artery catheterization The procedure has a number of advantages, including the following:
Minimal bleeding, a lower risk of nerve damage, a lower rate of complications, and a quicker recovery make the patient more comfortable because they can move around right away instead of spending several hours in bed. Before the procedure, an Allen test is used to evaluate the patient's hand's blood supply. The hand is supplied with blood by two arteries—the radial artery and the ulnar artery. If both arteries are functioning properly, then the catheterization procedure can proceed safely. Patients who are extremely thin or have arteries that are small or twisted are not candidates for this approach.
The following are the most frequently performed steps during radial artery catheterization:
A medication to help you relax will be given to you, and you will be asked to lie flat on the operating table.
To numb the wrist, a local anesthetic will be injected.
The radial artery is punctured with a thin tube known as a sheath.
The medication is administered via the tube to assist in relaxing the radial artery. The hand and arm may experience a brief burning sensation as a result.
Additionally, blood thinners are given to aid in the prevention of blood clots within the artery.
The catheters are then guided to the heart through the tube.
A coronary angiogram and stent placement may be performed if necessary.

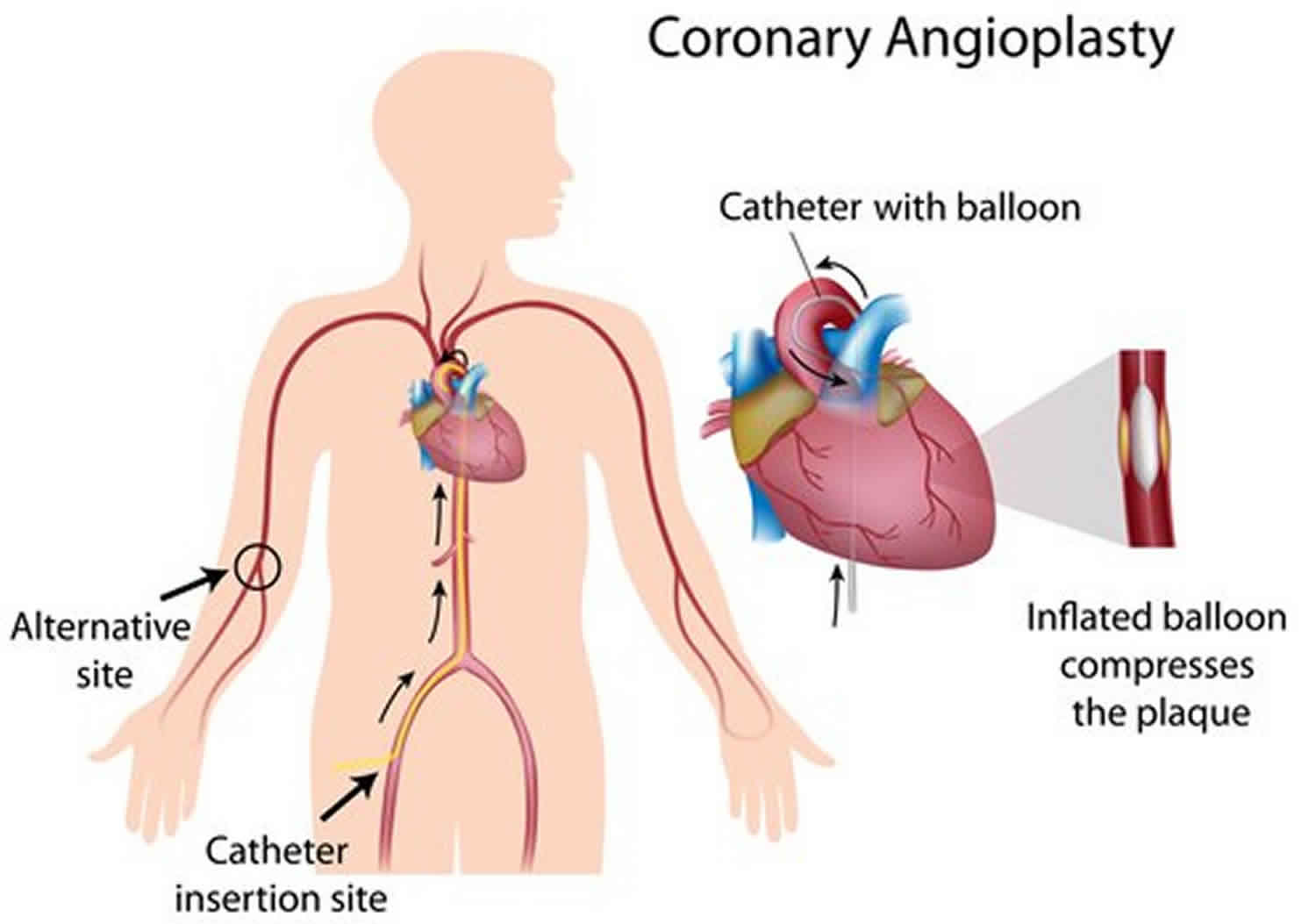
The inner walls of arteries, which carry oxygen-rich blood to all parts of the body, are typically flexible and smooth. However, plaque, which is made up of cholesterol, calcium, and fibrous tissue, can form on the inner walls of arteries, making them stiff, narrow, and hard. Atherosclerosis is the term for this artery hardening and thickening process. The part of the body that the arteries supply can suffer damage and pain as a result of atherosclerosis, which can either completely or partially stop the flow of blood through them.
The surgical procedure used to open up these narrowed or blocked arteries is called angioplasty. Your surgeon will inflate a small balloon inside the narrowed artery during angioplasty to widen it and increase blood flow. A stent, a tiny meshed tube that supports the artery wall and keeps the artery open, may frequently be inserted by your surgeon.
Local anesthesia is used for the procedure of angioplasty. X-rays are taken and a dye is injected into the body to observe the flow of blood through the arteries. Your surgeon will use these X-ray images to insert a thin guide wire through a blood vessel in your groin and use a small needle to extend it up to the blocked artery. The narrow tube known as a balloon catheter is then inserted through the guide wire into the blocked artery. At the tip of the balloon catheter, a deflated balloon is inflated at the site of the blockage. By pressing the plaque against the artery's wall, the balloon makes the artery wider. Along with the balloon catheter, your surgeon may also insert a stent, a wire-mesh tube, to keep the artery open and prevent it from narrowing again. The catheters and balloon are taken out, but the stent is left in place to keep the artery wide open and allow blood to flow freely.
Risks and complications This procedure rarely results in risks or complications. However, angioplasty-specific complications include:
re-stenosis (re-accumulation of plaque or scar tissue causing narrowing or blockage of the coronary artery; bleeding from the catheter insertion site; irregular heartbeat; chest pain during the procedure; damage to blood vessels caused by the catheter; damage to the kidney caused by the dye that was used with the angiogram; occurs within six months) blood clots and stent dislocation
The blood vessels that carry oxygen-rich blood to all parts of the body typically have an inner surface that is smooth and flexible. On the other hand, the deposits of cholesterol, calcium, and fibrous tissue known as plaque can accumulate on the inner walls of the arteries. The arteries can become hard, stiff, and narrow as a result of these plaques, reducing or stopping the flow of blood completely. Atherectomy is a procedure that can get rid of plaque.
The following narrowed arteries cannot be treated with Angioplasty and stenting, so atherectomy is recommended: procedure in which a thin tube with a balloon and/or a small mesh tube is inserted through a large leg artery to open up the obstruction Bypass surgery: Redirected blood vessels to avoid arterial blockage Atherectomy is sometimes used in addition to angioplasty and stenting. In this procedure, hardened plaques are first removed to some extent so that balloons and stents can be inserted, which widen the artery.
Local anesthesia is used for the atherectomy procedure. Using a small needle that is inserted into a blood vessel in the groin, a thin guide wire is inserted into the blocked artery. This directs a thin tube or catheter to the blockage, where a dye is injected and X-rays are taken to examine the artery's course.
After that, your surgeon will use a guide wire to insert an atherectomy catheter with a blade, grinding bit, or laser filament at its tip into the narrowed portion of the artery to remove the plaque. In order to remove significant portions of the hardened plaque, your surgeon may pass the catheter multiple times. The plaque is scraped off while it is in the collecting chamber or suction system at the tip of the catheter. Your surgeon will remove the hardened plaque and then insert a stent, a small mesh tube, into the artery to support and keep the wall wide open, preventing it from narrowing again. The catheter is removed after the treatment is finished.

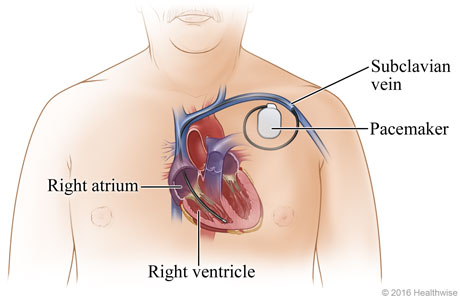
A muscular organ that circulates blood throughout the body is the heart. Electrical signals initiate the heart's rhythmic beating. The heart's rhythm can change if these signals change or are interrupted. A pacemaker is a small device that is inserted into the chest cavity to change the rhythm of the heart and keep it stable. A battery that can last anywhere from six to ten years, a pulse generator that helps analyze and regulate the heartbeat, and lead wires that stimulate the heartbeat make up a permanent pacemaker.
pacing device with one chamber: When the electric impulses traveling from the right atrium to the right ventricle slow down, which in turn slows down the heart rate, this kind of pacemaker is used. A single lead wire connects the pacemaker to either the right ventricle or the right atria.
Pacemaker with two chambers: Two lead wires connect this kind of pacemaker to the right ventricle and right atria, respectively. It keeps the heartbeat in check all the time and makes the heart pump more efficiently.